Last October, the Radio 1 DJ Adele Roberts announced she’d been diagnosed with bowel cancer. She’s been through intense treatment, and now wears a stoma bag as her bowel recovers.
Last October, the Radio 1 DJ Adele Roberts announced she’d been diagnosed with bowel cancer. She’s been through intense treatment, and now wears a stoma bag as her bowel recovers.
To hear her story and the sories from others on living with a stoma, click on the photo or here
Feedback from the Lewes Folk Evening – Sat 14th May

On Saturday 14th May we were treated to a brilliant evening’s entertainment at the Lewes Folk Club upstairs in the Elephant & Castle pub. The star attraction was “The Old Firm Plus One” comprising Marilyn Bennet, Iris Bishop, Denise & Stuart Savage and Jim Ward. Other acts were Charlotte Olive & Richard Spong and Martyn Wyndham-Read. The Lewes Folk Club pledged the gate money ( a not inconsiderable sum) to C-Side several of whose members were pleased to attend a thoroughly enjoyable evening.
Folk Evening in Support of C-Side – Sat 14th May
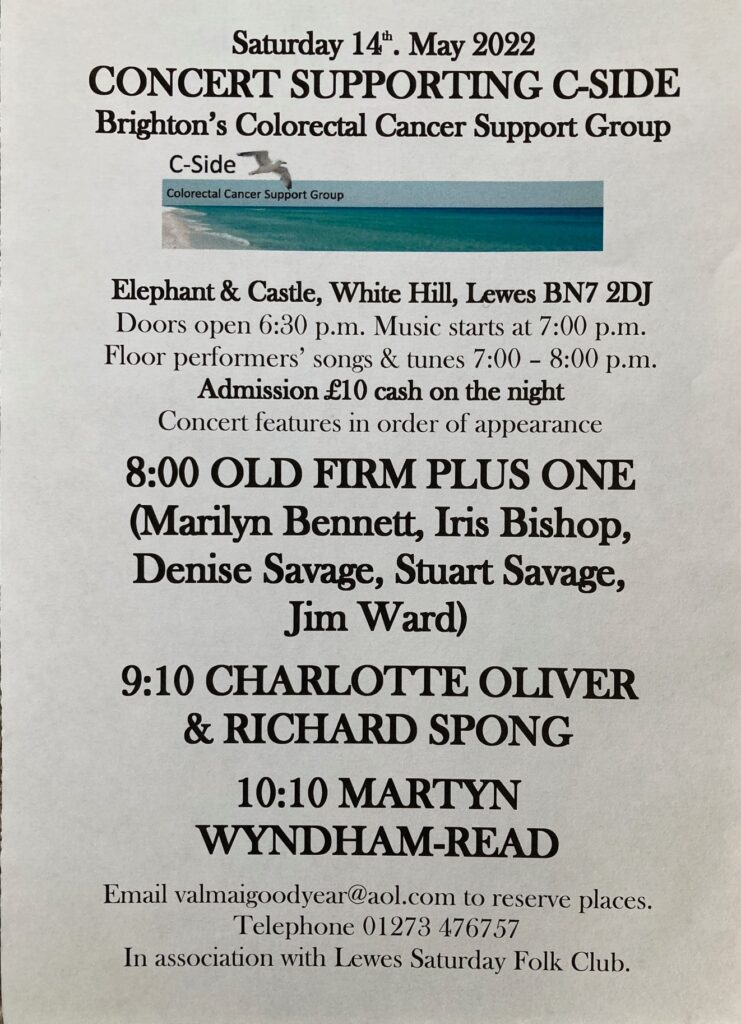 This is definitely an event not to be missed – a Folk Evening (long in the planning & postponed by the pandemic) in support of C-Side.
This is definitely an event not to be missed – a Folk Evening (long in the planning & postponed by the pandemic) in support of C-Side.
It’s all in the poster so get it in our diary. A great line-up of artists from the Sussex Folk scene.
To avoid dissapointment by being turned away or the discomfort of having to stand throughout this event, reserve a seat – see the email address on the poster
Nutrition Advice and Support from AITC
 C-Side has a great working relationship with Albion in the Community (AITC); over the years we’ve had many visits from their experts who have spoken to us on physical exercise & health matters. We were very pleased to welcome Mari Clark to our meetings on Thursday 24th January 2022. She gave us an interesting and insightful guide on nutrition and what consitutes a healthy diet; this being such a vital area of interest for all those living with bowel and anal cancer and other digestive diseases.
C-Side has a great working relationship with Albion in the Community (AITC); over the years we’ve had many visits from their experts who have spoken to us on physical exercise & health matters. We were very pleased to welcome Mari Clark to our meetings on Thursday 24th January 2022. She gave us an interesting and insightful guide on nutrition and what consitutes a healthy diet; this being such a vital area of interest for all those living with bowel and anal cancer and other digestive diseases.
To find out more of what Mari does click on the AITC logo above or on this link.
To learn more of Mari’s background and considerable experience go here.
Invest in the NHS Cancer Workforce
 Covid-19 exposed the terrible strain the NHS cancer workforce has been under for years. This is now the greatest threat facing the NHS. We are calling for the Government to use the Spending Review to fund the additional provision of NHS staff to diagnose, treat and care for cancer patients. Follow this link or just click on the image to read more and add your name to this petition:-
Covid-19 exposed the terrible strain the NHS cancer workforce has been under for years. This is now the greatest threat facing the NHS. We are calling for the Government to use the Spending Review to fund the additional provision of NHS staff to diagnose, treat and care for cancer patients. Follow this link or just click on the image to read more and add your name to this petition:-
https://petition.parliament.uk/petitions/596566
New drug could slow tumour regrowth in inoperable bowel cancer.
Adavosertib found to delay tumour growth in some patients in clinical trial, with few side effects
 Researchers have identified a potential new targeted treatment for incurable bowel cancer.
Researchers have identified a potential new targeted treatment for incurable bowel cancer.
The medication has shown promise in a clinical trial in slowing the regrowth of tumours among some patients with the condition.
The trial looked at whether a drug called adavosertib, taken as a daily pill, could delay tumour regrowth among patients with an aggressive sub-type of inoperable bowel cancer who have limited treatment options. Researchers compared 44 patients who took adavosertib with 25 patients who did not. They found that the drug delayed tumour growth by about two months on average and had relatively few side effects.
The drug had more effect in the 31 patients with left-sided/rectal tumours, increasing overall survival – meaning patients lived longer.
The lead author, Dr Jenny Seligmann, of the University of Leeds, said: “These results show promising signs that adavosertib may be effective in delaying regrowth of bowel cancer in some patients and is well tolerated.
“The findings are particularly encouraging as the subset of patients involved represent a third of all bowel cancer patients and, while other patients have treatments developed specifically for their tumour types, this group currently has very limited treatment options.”
The scientists caution that larger trials are needed to establish whether the drug improves survival compared with standard treatment.
The drug was trialled among patients on a treatment break after chemotherapy.
However, the research suggested adavosertib could benefit patients with other types of bowel cancer or alongside standard treatments in other lines of therapy. The subset of patients who took part in the trial had tumours with two common mutations, RAS and TP53. Scientists hypothesised these mutations would make the tumours more sensitive to the drug.
According to researchers, about a third of colorectal cancer patients have tumours with these two mutations.
In the UK more than 42,000 people are diagnosed with bowel cancer every year. It is the fourth-most common cancer in the UK and the second-biggest cancer killer.
The findings come from a large collaborative UK trial called Focus4 which aimed to investigate the best ways to help people with inoperable bowel cancer who have already received some chemotherapy. Co-author Prof Louise Brown, from the Clinical Trials Unit at UCL and statistical lead for the Focus4 trial, said: “The results for the adavosertib arm of the trial are potentially important and represent a glimmer of hope for patients in this group.”
Adavosertib kills cancer cells by inhibiting a protein that helps to regulate the process of cell division in the tumour.
Side-effects included fatigue, diarrhoea, neutropenia (involving low levels of white blood cells called neutrophils) and nausea, but none occurred in more than 11% of patients.
A second study from a separate part of the Focus4 trial called Focus4-N, also published in the Journal of Clinical Oncology, looked at outcomes among patients who had a complete break from treatment after chemotherapy.
They were compared with outcomes among those who continued chemotherapy using a simpler tablet called capecitabine.
Researchers found that, among those who had a complete break, the cancer started to grow sooner than in those on continued maintenance therapy.
But that maintenance therapy did not lead to an increase in how long people lived, the study suggested.
The Focus4 trial is funded by the EME Programme – an MRC/NIHR partnership – and Cancer Research UK and is run from the MRC Clinical Trials Unit at UCL in collaboration with Oxford University, Leeds University and Cardiff University.
Obesity Causes Cancer!
Watch this video to see how cancer (especially bowel and breast cancer) are linked to obesity.
The statistical evidence of this link is undeniable. This diagram gives a clinical explanation of the causal relationship:
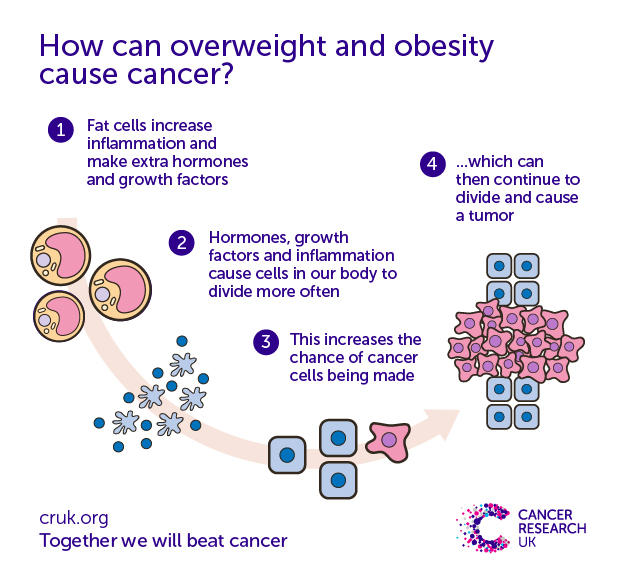 To read the complete Cancer Research UK article follow this link
To read the complete Cancer Research UK article follow this link
Old Man Cycling
 “My name is Mike. Over the years, our family has had help from a variety of charities, this is in a small way maybe turning the support the other way. How am I doing that? Bit of a bike ride. This is a long cycle, not sure how well that is going to go, and these charities are listed as potential beneficiaries. They all need support as recently charity fund raising has suffered.”
“My name is Mike. Over the years, our family has had help from a variety of charities, this is in a small way maybe turning the support the other way. How am I doing that? Bit of a bike ride. This is a long cycle, not sure how well that is going to go, and these charities are listed as potential beneficiaries. They all need support as recently charity fund raising has suffered.”
To read more, click on the image above which shows the charities that will benefit.
Mike is a member of C-Side and we wish him all the best for this mammoth test of endurance to take place on Sunday 19th June. Please find it in your hearts to make a modest sponsorship contribution. You can see that there are a wide range of beneficiaries, many of them might be of particular value to you one day!
To read more about the Chase the Sun event click here.
Swimming with a Stoma
 Gill Castle is on a mission to break down fear and stigma around swimming with a stoma bag.
Gill Castle is on a mission to break down fear and stigma around swimming with a stoma bag.
She proudly wears her colostomy pouch, which she needs following a traumatic childbirth – something Gill calls an “unspoken topic of conversation”.
To raise awareness of stomas and birth trauma, Gill has spent the winter months swimming in the sea off the coast of north-east England.
She told her story to BBC World Service’s Newsday. Click on the picture to watch the video.
Stoma Advice
 Long standing C-Side members will remember Helen Bracey, She was engaging, informative and an altogether outstanding guest speaker. Helen now works for Convatec and in their newsletter she describes eight top tips for maintaining healthy skin around your stoma :-
Long standing C-Side members will remember Helen Bracey, She was engaging, informative and an altogether outstanding guest speaker. Helen now works for Convatec and in their newsletter she describes eight top tips for maintaining healthy skin around your stoma :-
- keep stoma care routines simple – avoid using products on the skin containing perfumes, chemicals or anything else which may cause irritation
- always ensure your skin is completely dry before attempting to attach the baseplate of your stoma bag
- make sure your bag fits snugly and check the hole cut into your baseplate is the right size for your stoma
- check your skin regularly – even take pictures to help record changes
- if you notice output on your skin this could be a sign your bag isn’t fitted correctly
- a healthy diet can help towards healthy skin ask your GP for advice
- consider a barrier cream or adhesive remover if you don’t already use them
- as soon as you feel any soreness or itchiness around your stoma contact your stoma nurse
You can watch Helen giving this advice, in person, by clicking on this Youtube video link
Click on the Convatech logo above, to find out more about the company, its products and the information it offers to those with a stoma.
BSUH Stoma Care Service
It would be remiss to not mention here the excellent service that Kate Evans and her team provide within the NHS.
Click on this link to download the BSUH Stoma Care Service leaflet.